97
People
Number of people in A&E department
1:20
Hours
Average wait to be seen by a clinician
1:51
Hours
Average time in the department
Contact details
Triage Line 0118 322 7304
Address
Royal Berkshire Hospital
Craven Road
Reading
Berkshire
RG1 5AN
Related locations
Patient information leaflets
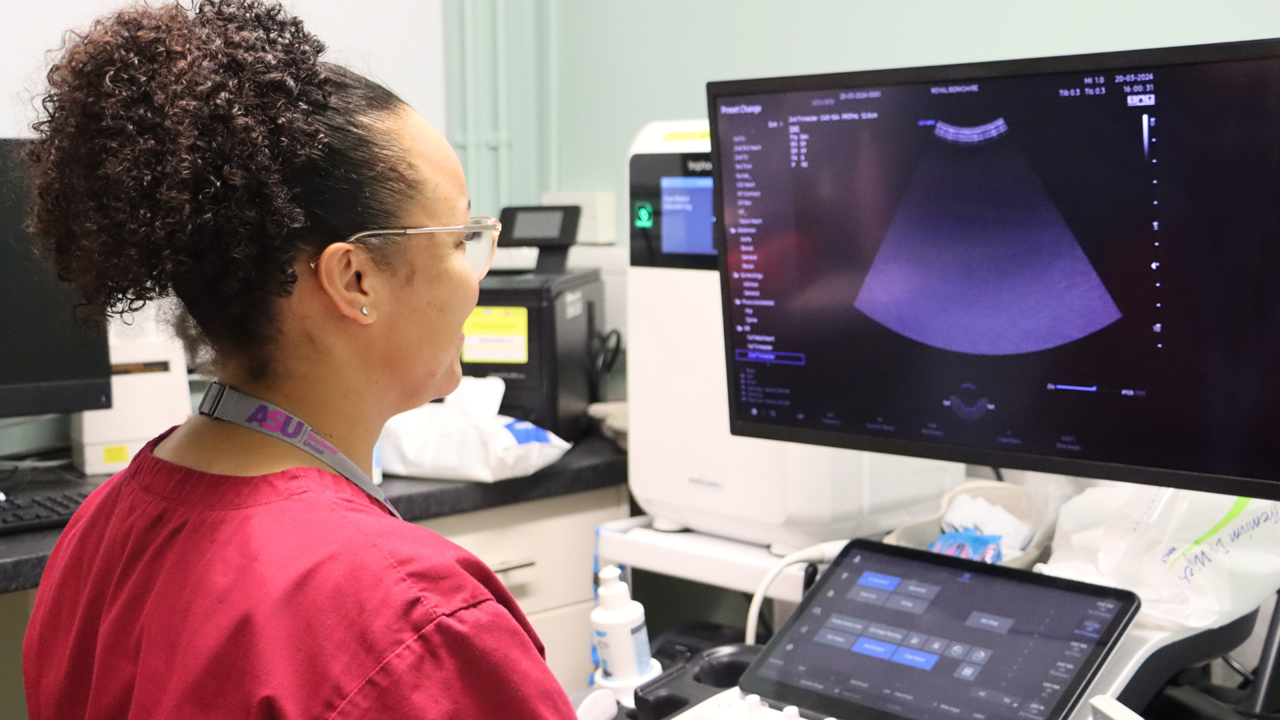
Royal Berkshire NHS Foundation Trust's Maternity services continue to be rated as Good by CQC
01 Mar 202407 Dec 2023
Related vacancies
Practice Educator Midwife - OASI and PPH Lead Midwife
Intrapartum Maternity Support Worker

Maternity
We provide personalised care for you and your baby, supporting you through your pregnancy journey, birth and early days of parenthood.
Booking your pregnancy care with us